Protocol - Retinal Digital Photography
Description
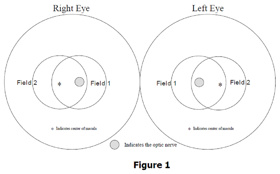
Two 45º digital retinal images (Field 1 and 2) will be taken of each eye of the participant using the Canon Non-Mydriatic Retinal CR6-45NM camera with a digital Canon D60 camera back (6.3 megapixels per image). Field 1 is centered on the optic disc and Field 2 is centered on the macula, providing photographic documentation of the optic disc, macula, and substantial portions of the temporal arcades. These photographs may be graded for retinal microvascular characteristics, including focal arteriolar narrowing, arterio-venous nicking, retinopathy (e.g., microaneurysms, retinal hemorrhages) and other conditions. In addition, generalized arteriolar narrowing is quantified using a computer assisted measure of retinal vascular caliber.
Specific Instructions
Training to take consistent gradable images is required although training is not extensive and quality of photography should be monitored throughout the entire study. Systematic grading of the images with adequate quality control procedures is imperative to minimize grader variability and to minimize misclassification leading to spurious or erroneous null findings.
This protocol uses the Canon Non-Mydriatic Retinal CR6-45NM camera with a digital Canon D60 camera back (6.3 megapixels per image). Other ophthalmic imaging cameras can be used. If other instruments are used, the reproducibility of the measurements should be comparable to those acquired with this protocol. The Ocular Working Group recommends cameras that capture images that are 5 mega-pixels or larger for use in grading and vessel measurement protocols. When other instruments are used to capture digital retinal images, the manufacturer and model of equipment should be recorded. These other cameras may require some different steps than are described in this protocol. Investigators should follow the equipment manufacturers instructions to ensure quality control.
In addition, this protocol uses EyeQSL,software which is commercially available through Digital Healthcare Inc. The Ocular Working Group notes that other ophthalmic imaging packages are available through other vendors that are similar in nature. These other software packages may require some different steps than are described in this protocol. Investigators should follow the manufactures instructions to ensure quality control. Please be sure to record the manufacturer and model and version of the software used.
Availability
This protocol is freely available; permission not required for use.
Protocol
Note: Example photographs A6, A7, and A8 referenced in the digital grading section of this protocol are provided and used with permission by the Atherosclerosis Risk in Communities (ARIC) Study Research Group.
Photography Protocol
1. EQUIPMENT SET-UP
The Canon Non-Mydriatic Retinal CR6-45NM camera equipped with a digital Canon D-60 camera back should be placed in a room that can be completely darkened during the photography procedure. This is because no dilating drops will be used and we rely on the natural dilation of the pupil that occurs in the dark to perform the fundus photography. The camera should be placed in the room so that the patient has easy access to the examination stool and so that the photographer has ready access to the room light switch. A small reading lamp located near the camera may be used to help the photographer see to navigate and write during the procedure. This lamp should be turned off during photography to reduce the risk of pupil constriction. Light from the computer screen may need to be adjusted to minimize pupil constriction.
The fundus camera will be set on the motorized instrument table and the laptop computer will be attached to the articulating arm located above the cameras video display monitor. The pneumatic stools are positioned on opposite sides of the fundus camera.
1.1 Daily Set-up Procedure
The camera dust cover and lens cap should be removed at the beginning of the day and the lens inspected and cleaned (see section 1.2) as necessary. Dust is the greatest enemy, producing the majority of artifacts on the photographs. When the camera is not in use, the lens cap should be in place and the special dust cover must remain on the camera.
1.2 Camera Lens and Body Care
Before each photograph, the camera lens must be inspected and, if dirty, cleaned with the brush and air bulb to remove debris. Should more extensive cleaning of the lens be required, the lens can be fogged with your breath or moistened with absolute alcohol and then cotton should be used in a circular polishing motion until no dirt or oily film is visible on the lens when it is viewed from the front with the alignment lens removed and the view lamp on and turned up to its near maximum intensity (see page 28 in the Canon Non-Mydriatic Retinal Camera CR6-45NM Operation Manual). The body of the camera should be kept clean and free of dirt with a soft cloth and water or a common spray cleaner. The forehead rest may be cleaned with alcohol.
1.3 Flash, View and Split Lamp Concerns
The Canon cameras are equipped with new lamps at the beginning of the study. It is not anticipated that the flash, view or split lamps will fail during the study. The view and split lamp should last approximately one to two years and are easily replaced as needed. The flash lamp has a life of at least 5,000 flashes. Since the view lamps are relatively inexpensive bulbs, one spare should be ordered from Canon USA, Inc. and kept at the field center. Clinic staff in the field can replace the view lamp. Remember to keep all oil from your fingers off these lamps during replacement. The flash and split lamp should be replaced by a qualified technician. Both lamps can be ordered from Canon USA, Inc. when needed for overnight delivery.
As the flash lamp ages, the light output can diminish, producing progressively darker photographs. This can temporarily be over-ridden by an adjustment of the transformer output, though ultimately the lamp should be replaced. The flash lamp requires careful handling during installation (the burnt out lamp may be hot, and the new lamp must be properly aligned. Replacement should be attempted only by staff trained to do this.
2. SUBJECT PHOTOGRAPHY OVERVIEW
Digital images will be captured into a table mounted laptop computer, archived to CDs for analysis. Before the first patient of the day is photographed, the photographer prepares the camera by first turning on the power to the Canon D-60 camera back. The power is then turned on for the Canon Non-Mydriatic Retinal CR6-45NM camera and to the Dell laptop computer. The photographer escorts the patient into the photography room, positioning them before the fundus camera, and explains the procedure. The EyeQSL software program is initiated and subject ID and photographer information is entered into the appropriate computer screens and the software is set to acquire images.
Patients will have one eye assigned as the study eye and the other eye assigned as the
fellow eye. Photography will be performed of both eyes with the study eye photographed
first. All subjects will have two 45-degree photographs taken of each eye. The first photograph will be centered on the optic nerve and this is referred to as Field 1. The second photograph will be centered on the macula and will be referred to as Field 2. A diagram of the location of these two fields can be seen below in Figure 1. The images are stored on the hard drive of the computer as the procedure for the first patient is ended and the camera is prepared for images acquisition of the next subject. At the end of each week, the images are archived to CD.
The study eye will be selected based on the subjects ID number. When the sixth digit of the ID number is even, the right eye will be photographed first, and when it is odd; the left eye will be photographed first. If the eye specified by this algorithm is considered too difficult to photograph with adequate photographic quality, only the opposite eye should be photographed, and an explanatory note entered in the MESA Photography Completion form. Conditions falling into this category are (based upon the technicians judgment): eye missing, inability to dilate at least 4 mm, inability to fixate adequately for proper photographic fields, and opacities of the media preventing a reasonably clear view of the retinal vasculature and resulting in unreadable digital images.
2.1 Subject Exclusion
The photographer will attempt photography on subjects with poor visual acuity who may be unable to direct their gaze so that their optic nerve or macula is properly positioned on the camera monitor (as may be the case where both eyes are blind or when the subject is deaf and communication with them is impossible). In these cases, the photographer should get the best field definition possible. If, in the photographers judgment, no acceptable photograph can be taken of either eye, the subject will be excused from photography.
The photographer should attempt photography on those subjects who are physically disabled, to the point that they can be comfortably positioned at the camera. To facilitate this, the subject may remain in a wheel chair positioned before the motorized camera table lowered to the appropriate height. Care should be taken when lowering the camera table to avoid pressing against the subjects legs. If, in the photographers estimation, the subject cannot be comfortably positioned, no photography will be performed.
2.2 Subject Explanation
Photography begins with a complete explanation of the procedure to the participant by the photographer. A color illustration may be useful to show what the retina looks like. It is important to reassure the subject that no retinal damage is caused by this procedure. The subject should know to expect several flashes. The pictures will include the macula (area of central vision) and it is normal to experience a blue or red tint to vision immediately following the flash. This disappears within five to seven minutes. No dilation drops will be used for this examination, and the eyes will not be touched. A sample script of a typical retinal photography explanation (suitable for use as written material for deaf or interested subjects) follows:
We will be taking several photographs of the inside of the back of both of your eyes (the retina) so we can study the blood vessels and look for any unusual changes. We will not be touching your eyes or be giving you any eye drops to take the pictures. Instead, you will be asked to sit in a darkened room before a special camera with your chin in a chin rest. We darken the room so that your pupils will dilate and we can align and focus the camera on your retina. While your pupils are dilating, we may ask you some questions about your vision and the health of your eyes. During the aligning process you will only be aware of some small red lights and a blinking green box and red bars visible in the camera lens. We will ask you to follow the blinking green box as we move it. Just before we take the picture, we will ask you to blink your eyes and then open them real wide. The camera will flash a light from within the camera lens as each picture is taken.
Just after the picture is taken, you may see a blue or red circular spot before the eye photographed. This will disappear within 5-7 minutes and causes no damage to the eye. Please remember that we are only taking pictures (not an x-ray) of a small portion of the back of your eyes and that this picture will not substitute as an eye examination. You will certainly be notified should we notice anything requiring immediate attention. Please continue to see your eye doctor on a regular basis for your complete eye examinations.
2.3 The Photography Completion Form
The Photography Completion Form records the circumstances of the photographic session, and can only be completed as the session begins. The participants ID# and acrostic will appear at the top right hand corner of the form. The sixth digit of this number will determine the study eye (right eye if even, left eye if odd); this eye should be photographed first. Before beginning the photography session, the photographer records the site number, photographer ID#, and the photography date. If either eye cannot be photographed for a reason gathered during the ophthalmic history (e.g., that eye has been enucleated) or for a reason that emerges during the first part of the session (one eye does not dilate sufficiently well to be photographed), the photographer should record this on the form. The flash setting (2 unless re-adjusted by the photographer) and the estimated diameter of the pupil at the time of the first photograph of each eye should be recorded. The photographer is encouraged to comment on anything unusual such as artifacts, pathology or other problems encountered during the session. When the photography session is over and the photographer is reviewing the images in the contact strip, the eye and fields photographed should be marked. If extra images were taken, mark other and record the reason for extra images in the comments section. When the final images for each have been decided upon by the photographer, he/she can record the total number of images taken of each eye. Photocopies of this form will be mailed along with the images for analysis.
Please see Photography Completion Form2.4 Preparing the Camera
The Canon D-60 digital camera back must be turned on first. This is done using the small dial located on the back left side of the camera body. This must precede turning on the Canon fundus camera or computer since the camera "looks" for the D-60 camera body during start up. The Canon CR6-45NM video display is activated when the power switch on the side of the main unit is turned on. If no photography or switch operations are performed for 10 minutes, a power saving mode is activated, turning the lamps and display off to prevent unnecessary wear. During this power saving mode a green "ready" lamp blinks on the monitor. Pressing any button below the monitor will reactivate the system.
Notice that the flash power setting (located on the lower right-hand corner of the monitor) blinks when the main unit is switched on. This indicates the system is charging up. Do not attempt to take photographs until the blinking stops, indicating a fully charged flash.
The camera contains an internal clock and the date will automatically change each day. The photographer must manually change the date if this clock should fail or if the camera is left unplugged for a long period of time. The date is displayed on the fundus camera monitor and is changed through the menu located in the "Set 3" screen (see pp. 18-20 in the Canon Non-Mydriatic Retinal Camera CR6-45NM Operation Manual). The date format will read Month-Day-Year. The display form "Disp Form" screen ("Date" subscreen) is used to adjust the current date.
The Canon D-60 camera body should be attached to the main unit and set with the following settings:
Shutter speed: 60Mode Dial: Manual
AF-WB: Flash
Quality: First Level Large
Red Eye: Off
AEB: 0-
ISO: 400
Beep: Off
Auto power off: Off
Review: On
Review Time: 8 seconds
LCD: Normal
* The camera should remain ON until the end of the day
3. EXAMINATION PROCEDURE
3.1 Subject Positioning and ID Entry
The subject and photographer are seated on the appropriate sides of the retinal camera. The subject is positioned so that he/she is comfortable with chin and forehead in the headrest. Chin height should be adjusted so that the eyes are approximately level with the height adjustment mark on the face rest pole. The room is darkened to the level where a newspaper can barely be read (equal to about 5 lux) and the camera room door is closed. The only light in the room should come from the display monitors. If a lamp is used to aid the examiner during administration of the questionnaire, it must be turned off when photography is performed.
While the subject begins to dilate, the photographer begins the image capture procedure by double clicking the desktop Digital Healthcare Client icon and selecting the EyeQSL program. A "Login" screen will appear in which the name and password that has been setup for that computer are entered. An "Unarchived Visits" screen will appear and will contain images from any patients who have not yet been archived. Select the "Next" button on this screen to open the "Identify a Patient" screen. The photographer then enters the patients subject ID number in the Patient Number. The subjects last name and first name are not used to preserve subject anonymity. The first six letters of the acrostic (name code) and photographer ID# should be filled in the appropriate boxes. These fields must be filled in before the photographer is able to begin capturing images. Additional information may be entered into fields as indicated in the study protocol. The "Next" button is clicked until the "Confirm Patient number" box appears, at this point, the patient number is re-entered and the "OK" button is selected. A "Visual Acuity" box will appear, click "Cancel".
The photographer is ready to begin taking photographs when the 4-panel split screen and timer box appear. The timer box displays the time the photograph was taken and also the current photo number.
When the photographer takes a picture, the timer stops and the image will briefly appear on a screen located on the digital camera back. It will then take a few seconds for the image to transfer from the camera to the computer screen. The timer will restart after the image appears on the screen. The photographer will review the image for quality and may take another image if they believe a better quality image can be obtained or they may accept the image by simply taking the next photograph when the patient is ready and the pupil is adequately dilated.
At the time the photographer has completed the patients photographs, he/she will select the "End" button located on the timer box. The photographs that have been taken will then appear on the computer screen in a "Contact Strip" box. The photographer reviews all of the images in the contact strip and may delete any unwanted images at this time. This is done by left clicking on the image to be deleted, making the gray border around the image turn purple. Select "Delete from..." on the menu that appears. Select "Delete from Visit." The photographer may then elect to continue the photography session, if they wish to retake a particular field. Once the technician is satisfied with the photographs, he or she can select "Quit" to end the photography session. At this point, a new subject may begin being photographed by filling in the new patient information and repeating the steps stated above. If no other participants are to be seen, the photographer can "Quit" the program.
3.2 Pupil Size and External Camera Alignment
The camera stage holding knob is unlocked, the alignment switch is turned on and the stage is moved to center the eye to be photographed horizontally and the height adjustment ring is used to position the eye vertically. The pupil should appear on the TV screen coincident with the central circle on the monitor. The camera joystick is moved forwards or backwards until the pupil appears perfectly round. At this point, proper external alignment has been achieved. A pupil larger than the central 4mm circle on the monitor is required for adequate photography. If the eye does not dilate to at least 4mm after a 5-minute waiting period, the fellow eye should be examined for pupillary dilation as well. If dilation of the fellow eye is larger, the photographer will photograph the fellow eye first. At this point, the pupil size is measured using the alignment circle on the monitor as a gauge. This measurement is estimated to the nearest 1mm and it is recorded on the Photography Completion form.
3.3 Internal Eye Alignment
Once proper external pupil alignment is achieved, the alignment switch is pressed to provide a view of the fundus, split focusing lines, corneal reflection dots, and the fixation light. If no split lines are seen, the height or left/right adjustment is improper, the "Split" (split lines) setting is set to "off" (Set 1, Split/FCD), or the diopter compensating slider is pulled out. The split lines may fade in and out if the pupil is too small, the alignment of the camera is not centered on the pupil, or if the eyelashes or lids eclipse the light. If no corneal reflection dots are seen, the forward/backward adjustment is improper. The best photographs are obtained when the eye is well dilated, fixation is on the target; and lids and lashes are held wide open.
3.4 Alignment, Focus and Proper Fixation of Fundus Photographs
While viewing the fundus image on the screen, the photographer carefully adjusts the fixation target control button to locate Fields 1 and 2 correctly on the screen. Field 1 is always photographed first.
Any fine adjustment of fixation is made by moving the fixation lever and instructing the subject to look into the lens of the camera at the green target box. In the event that the subject sees no fixation light with the eye being photographed, the photographer must carefully instruct the subject to make micro movements (fine movements up, down, left or right) until the protocol fields are located.
Once the fixation is confirmed, the photographer must constantly adjust and position the camera to maintain the correct position of the corneal reflection dots. It is important that these dots be properly positioned at the three and nine oclock positions before the picture is taken. This will ensure the correct distance from the eye and will allow capture of a sharp digital image. Focus is done manually by dialing either of the focus knobs located on the side of the fundus camera. Proper focus is obtained by aligning the two horizontal focus bars visible on the fundus camera monitor (see p. 12 of the Canon Non-Mydriatic Retinal Camera CR6-45NM Operation Manual). Good focus is critical for grading photographs.
The photographer will instruct the subject to blink once or twice just before the picture is taken. This blinking will insure a moist (and subsequently clearer) cornea and will safeguard against unwanted blinks at the moment of exposure. Once alignment is satisfactory, the shutter release, located in the tip of the joystick, is depressed and the exposure is made. The quality of the digital image is evaluated by the examiner and ungradable images, which in the opinion of the photographer may be improved, may be retaken. Once the best quality image is obtained, the second field is photographed and the photographer conducts the same image evaluation procedure.
4. PHOTOGRAPHIC CHALLENGES
4.1 Photography Through Small Pupils
The photographer will experience much more difficulty attempting photography through small (less than 4mm) pupils because all of the camera light doesnt enter through the smaller pupil. This usually results in uneven illumination (seen as dark shadows) on the monitor. In this situation, the photographer must make careful camera adjustments to position the shadows as far away from the optic nerve in the Field 1 photo and away from the macula on the photo of Field 2.
A small percentage of subjects eyes will not dilate to the minimum 4mm required for adequate photography. Certain medication may prevent any dilation and the pupil size observed on the monitor may be 2-3mm, inadequate for the photographer to appreciate all retinal landmarks on the viewing monitor. In this case it is recommended that the photographer introduce the small pupil aperture located on the left side of the fundus camera body (see p.10 of the Canon Non-Mydriatic Retinal Camera CR6-45NM Operation Manual). This function adjusts the illumination to concentrate more of the retinal illumination into a smaller area providing more even illumination to the center of the field while sacrificing illumination at the field perimeter. If after introducing the small pupil function only one focus line is visible, it might be necessary to adjust the camera position either vertically or horizontally to bring the second line into view so that accurate focus can be set. However, there may be circumstances that prevent the second line from appearing, even when the camera adjustments are made. In these cases it may be helpful to remove the small pupil function momentarily while searching for the second line and adjusting focus, reintroducing the small pupil function before taking the photograph.
If no retinal landmarks are visible, often the case with ≤2mm diameter pupils, the photographer should adjust the camera slightly to position the corneal reflection dots slightly above or below their optimum position. This technique allows a portion of the illumination light (which falls on the iris when the pupil is small) to enter the eye. If any retinal landmarks become visible with this technique, a picture should be taken. However, if no retinal landmarks are visible, no picture is taken. The photographer notes the problem on the Photography Completion form.
4.2 Exposure Compensations for Dark or Light Retinas
The normal flash output used in this study will be flash number 2. The flash output can be increased or decreased by first pressing the "DA" button followed by the +/- buttons located under the main video display screen of the fundus camera monitor. Higher numbers increase flash output and produce brighter images while lower numbers decrease flash output and produce darker images. A one number increase or decrease in flash intensity is usually all that is needed. Photography through small pupils, media opacities or of darkly pigmented retinas (Black or Asian) will require increased flash output (to flash 3) to avoid underexposed pictures. Photography of lightly pigmented retinas (blond, albino or Scandinavian) will require decreased flash output (to flash 1) to avoid overexposed pictures. The photographer should check the color saturation of the first image taken of each participant, and adjust the flash if necessary before proceeding.
4.3 Focus with High Myopia or Hyperopia
The diopter compensation slide should be set to the "0" position for most eyes. This is the only setting in which the focus bars are active and allows photography of eyes with refractions between -12 and +15 diopters. In the event that the eye photographed falls outside this range and focus cannot be achieved, as in the case of aphakia or high myopia, the diopter compensation slider must be adjusted for the clearest focus to the "+" or "-" position and the focusing knob is then turned manually to provide the sharpest image as seen on the monitor. Obtaining a brighter retinal image by increasing the view light intensity can facilitate this. The normal setting for the view light intensity adjustment is approximately 4.
Standard TV monitor functions can be adjusted for the photographers viewing comfort (including contrast and brightness) by opening the access door below the TV monitor. These are standard controls similar to those found on a home TV set and only effect viewing; they do not affect final photo quality.
DIGITAL GRADING PROTOCOL
The photograph grader views each retinal image with a high resolution monitor using the EyeQ Lite image processing software and database, and references the written protocol and the digital photographic standards and examples to evaluate retinal abnormalities. The photograph grader directly enters his/her evaluations in a micro computer database.
1. USING THE IMAGE PROCESSING SOFTWARE/DATABASE
1.1 LOGGING IN
To access the image processing database the grader will double click on the Digital Healthcare EyeQ grading icon on the desktop. The grader will then be asked to log into the database. The login is the same for all workstations with the both the user name and password case sensitive). Then the grader selects OK from the login screen.
Login: Name:Password:
Select OK
1.2 SELECTING A PATIENT VISIT FOR VIEWING
The first screen to appear is the Identify a Patient screen. The grader may type in the Study ID # of the patient to be reviewed and then click on Next. The database will find any patient visits with that study ID and display a list of visits with their corresponding study dates in the Patient Found in Database menu. Double click on the patient visit to be viewed. A final menu called Select Visit/Study will appear. Again double click on the visit to be viewed. A "contact strip" of 4 or more images will appear. This contact strip should contain field 1 and 2 of both eyes. (Additional images may be present.)
To select an image from the Contact Strip for further viewing or measurements either, right click on that image and the image will enlarge to full size (left clicking on the image (a purple frame will appear around the selected image) and selecting view image from the side bar menu will accomplish the same thing). Note: The title of the sidebar menu is helpful to remember in negotiating through the software.
1.3 IMAGE MANIPULATION TOOLS
There are many image manipulations available using the EyeQ software. Change in magnification, various manipulations of contrast, and splitting the image into the separate red, green and blue color channels are among the most commonly used. Further descriptions of the EyeQ software can be found in the users manual.
The manipulations that will be performed on all images before measurements are performed are listed below in order. After each manipulation the image should be returned to its normal state before starting the next manipulation. If at any time the grader notes a suspicious area in the image the grader may zoom in/out and/or lighten/darken to enhance the area of concern
Zoom In (or Zoom Out): This will magnify the entire image for viewing. Magnifying the image two times at most is usually adequate (available on the View Image Menu). To magnify a localized area of the retina (to closely examine retinal vessels or specific lesions or color changes) the grader can left click on mouse when the magnifying glass is displayed. This can be done at any time during image manipulation even after a complete zoom has been performed. Another method for zooming in is to use the scrolling wheel on the mouse. This can be done at any time.
Lighten (or darken): (This option is available in the contrast menu only.) When an image is particularly light or dark this function is very helpful. One or two clicks is adequate to allow better viewing of poorly illuminated areas of the retina (similarly for overly exposed retinal images and darkening).
Image Manipulation Steps for all images:
1. Zoom in (lighten/darken/stretch as needed)
2. Red-Free (or 3 RGB components) (stretch lighten/darken as needed)
Optional steps if above steps demand more manipulations
3. Equalize Histogram
4. Invert image
5. Median ≥ 128
View Image Menu
1. Red-free or RGB color option: This provides the grader with a full screen view of the green channel. The grader should select Zoom In (or Zoom Out) and left click on the mouse to magnify a given area, and scan the entire photo. After magnification the grader should select the Contrast submenu, and Lighten (or darken), and/or Stretch the image for another view. (Again, suggest manipulating the image two times at most). To return the image to its normal state, click Undo to negate the lightening (or darkening) of the image and return grader to the original image. (Instead of choosing the Red-free option, the grader can view all of the color channels (red, green and blue) by selecting RGB. This will display a montage of the color image and each of its color components. The 3 color channels can be split and saved back to the contact strip for additional manipulations or measurements (lighten/darken, zoom in/out, stretch, etc) or the entire montage can be save as one image to the contact strip. It should be noted that saving these images is only temporary, remaining intact only while the grader has that patient file open. This montage is helpful in gauging areas of overexposure in the red channel, among other things.)
Contrast Menu
This menu takes the grader to a submenu of options for increasing contrast of an image. All manipulations are temporary and will never overwrite the study images. If the grader wishes to restore the image to its original state they should select Undo. If the grader wishes to perform additional manipulations or measurements on the image that are not available in the Contrast Menu then the grader should select Quit and Store. This will return the manipulated image to the contact strip. When the grader quits this patient visit, the contact strip will return to the original study images only.
2. Equalize histogram: This function examines the distribution of levels and redistributes them as evenly as possible across the range from 0 to 255 in all three channels. Values of pixels are changed so that an equal number of pixels have each of the possible levels. Thus, details in areas that are particularly bright, where there are many pixels at a similar brightness, are seen clearer. While this function dramatically shifts the colors of the image when combined with Lighten/Darken, it is often quite helpful in detecting small color changes, drusen or microaneurysms.
3. Invert image: This function alters every pixel so that its grey-level, initially G, becomes 255 - G. This reverses the gray scale or in the case of color image, reverse each color channel. The operation works over the window selected in the processing menu. If the range option is in the menu and the limits shown by it are not 0 and 255, the contrast is inverted linearly within the narrower range. Pixels with grey levels less than the minimum range limit are all set to 255. Pixels with grey levels greater than the maximum range limit are all set to zero.
4. Median ->128: This option determines the median grey level, then scales the grey levels so that pixels at median value get a level of 128 (halfway between 0 and 255).
Contact Strip Menu
Grading Tools and Grids
After all standard manipulations are performed on the study images for the eye the grader is ready to perform measurements using the Macular Grid, Neovascular or Optic Nerve Grid and Measure Lesions found in the View Image Menu under Grading Tools. Any measurement performed can only be done on the original color or the red free image. Stretching, Lightening/Darkening and Zoom In/Out are the only acceptable manipulations during the measurement session. Measurements may not be performed on any other type of manipulated image.
Before any measurements the grader should confirm that the disc diameter calibration measurements are correct. To do this the grader selects the Grading Tools option, and confirms that Measure disc diameter is 346.7 (the number of pixels in a standard disc diameter) for a Canon D60 Camera. (For a Canon D30 Camera the measurement should be 243.8 pixels for a standard disc diameter and for Canon 20D the measurement is 395.2 pixels for a standard disc diameter.) If 0 or an incorrect measurement is shown, then grader selects Enter disc diameter pixels, and inserts the correct measurement, then selects OK.
There are two grids available to the grader for use in areas of measurement. The grids, were developed for use with Canon 45? retinal photographs, are based on the diameter of an average optic disc as calculated by comparing Zeiss 30? and Canon 45? photographs of the same eye from several individuals and appropriately scaling down from the standard disc diameter (DD) for Zeiss 30? photographs.
Neovascular or Optic Nerve Grid: The first grid is the optic nerve grid. The optic nerve grid will be used for grading both new vessels on the disc and for defining the 4 quadrants evaluated for arterial narrowing and A/V nicking. The grid consists of three concentric circles centered on the optic disc and four spokes at 12:00, 3:00, 6:00 and 9:00. The inner circle approximates the disc margin assuming an average size disc (diameter = 1 DD or one disc diameter, radius = 1/2 DD); the second circle demarcates a zone extending to 1/2 DD from an average disc margin (radius of circle = 1 DD), hereafter referred to as Zone A; and the outer circle demarcates a zone extending from 1/2 DD to 1 DD from the disc margin (radius of circle = 1 1/2 DD), hereafter referred to as Zone B. The four spokes extend outward from the edge of Zone A and demarcate the four quadrants named for their relationship to the posterior pole (the most posterior retinal region which contains the optic disc and the macula, or center of acute vision). Beginning at the upper left and moving clockwise, the four quadrants in the right eye are the superior temporal, superior nasal, inferior nasal and inferior temporal; in the left eye, the superior nasal, superior temporal, inferior temporal and inferior nasal.
Macular Grid: The second grid to be used is the macula grid. This grid will be placed over the center of the macula to define the macular area for grading of Age-Related Maculopathy (ARM) and for Clinically Significant Macular Edema (CSME). It consists of 3 concentric circles with diameters of 1000 microns (.6666 DD), 2 DD and 4 DD and has 4 radiating lines from the central circle radiating out at 1/4 hours (1:30, 4:30, 7:30 and 10:30). The grader will left click on the mouse to position the grid in the center of the fovea, then release the mouse button to "drop" the grid onto the image. Once centered, the X and Y coordinates of the center point, or the fovea, should be recorded for future grid placements. Once placed on the image, the grid can be tilted or adjusted by using Meridian angle 0 degrees.
Meridian angle 0 degrees. This option adjusts the tilt of the macular grid. Left click, and select the location on the image where the horizontal line will cross the optic nerve (Right eye at about 7:30, Left eye about 4:30 on the disc margin). This X and Y coordinates of the first point will need to be recorded for future grid placement. For the second point, plug in the X and Y coordinates saved from the macular grid placement earlier (center of the macula). The grid should rotate into the correct position.
Measure lesions. This measurement tool is used primarily for measuring drusen size and area. The grader can size lesions using the circle sizes ranging from Co (comparable to 63 microns diameter) to 1 DA/DD (a circle of 1500 microns in diameter). Right click on the mouse for ascending order in size; left click for descending order. By using the center scroll wheel the image can be zoomed in and out during measurement.
2. GRADING PROCEDURES AND RULES
2.1 GRADING CONVENTIONS
All sets of participant images are assigned a sequential reading list (five participants per list) as the images are received at the Reading Center. The grader selects a reading list from the coordinators tracking binder at the beginning of a grading session. Upon completion, the grader initials and dates the tracking sheet and forwards the list to the appropriate basket provided for completed lists.
Photograph graders at the Reading Center use the following conventions in evaluating the presence and severity of abnormalities:
a) None is used to indicate that a lesion is absent. If there is a suggestion that a lesion may be present, but the grader is less than 50% certain that the lesion is in fact present, the grader uses none, or absent, for that lesion.
b) Questionable is used to indicate the probable presence of the lesion. If the grader is more than 50% certain but less than 90% certain that the lesion is present, he/she selects questionable as the answer. Stated alternatively, if the grader thinks that the lesion is present but is unsure that all observers would agree, he/she marks the lesion as questionably present.
When an abnormality is present but the grader is uncertain of its identity, the grader chooses questionable for the lesion considered most likely and answers none, or absent, for the lesion(s) considered less likely.
c) Definite indicates the definite presence of a lesion. If the grader is at least 90% certain that the lesion is present, he/she marks the lesion as definitely present.
d) In questions with several codes for definite presence of the lesion, there may be several steps to indicate ascending severity of the lesion. The ascending severities may be described in general terms as mild, moderate and severe. The severities of a lesion are usually defined either in terms of the number, length, or area present, or in relation to photographic standards.
e) Cannot grade is used to indicate that the lesion is ungradable due to impaired photographic quality or a confounding condition. In general, if no evidence of the lesion is seen and more than 50% of the area of measurement (subfield, grid area, quadrant etc) is missing or obscured, the grader selects cannot grade rather than none. Cannot grade is also used where the area of measurement is present and unobscured but impaired to a degree that the typical appearance of the lesion in question could not be identified. For focal narrowing of arterioles in the quadrants, at least 1 1/2 DD total length of arterioles should be visible in the quadrant; if no abnormality of the arteriole is seen and less than 1 1/2 DD of arterioles are available for assessment, the grader selects cannot grade as the appropriate answer. (In judging A/V Nicking, if no arterioles cross over veins (only veins crossing over arterioles) then None is the appropriate grade.)
If a specific lesion can be seen in any part of the field, it should be assessed as such even if the remainder of the field is ungradable.
f) Lesions occupying more than one quadrant are assessed as present in each quadrant and the number, length, or area involved is estimated in each quadrant separately.
2.2 GRADING SYSTEM
The grading system includes a preliminary and detailed grading followed by a photograph edit and adjudication if necessary. Each set of images will be graded on the items detailed below using custom designed computer software with built in completeness and consistency checks Upon completion of this detailed grading, a comparison will be made between the preliminary grading and the detailed grading. If there is a disagreement in the levels assigned for specific lesions, the eye will be sent to a third grader for an edited grade of those lesions. If the edited grade still does not agree with either the preliminary or detailed score, then the eye will be sent to the consulting ophthalmologist for adjudication.
3. THE GRADING FORM
The data collection form exists in both an original paper format and as a direct entry screen. In both, the data collection begins with identifying information and is followed by the collection of substantive grading data.
The identifying information (participant identification number, photo date, and name code or acrostic) is entered first. In direct entry, the grader must correctly enter the participant identification number, photo date, and name code, which are then checked against the photograph inventory, before entering data for the eye. The direct entry software does not permit data entry for an uninventoried identification number, and shows the grader if data are already present for the identification number.
Some items such as Arterial Changes, ARM lesions, Other Vascular Lesions or Any Other Lesions, are organized under gatekeeper questions. The gatekeeper for each eye asks the grader if any arterial changes (ARM Lesions, Other Vascular Lesions, etc) are questionably or definitely present in the eye, or ungradable. If yes (code 2), the grader completes all items specific to that group. Comments are used to describe other abnormalities not listed in the grading form, or to provide additional details for items graded.
Please see Grading Form
3.1 PRELIMINARY GRADING
The purpose of preliminary grading is four fold: to provide immediate pathology notification to the participant and his/her primary eye care provider, to provide timely image quality review and feedback to photographers, to provide an overview of the health of the eye for general feedback letters, and for purposes of editing. The items to be evaluated are detailed below.
3.1.1 QUALITY GRADING
Field 1 and 2: If field 1 photograph is present, the grade is "Present", code=2. If the field 1 photograph is absent, the grade is "Absent", code=0. If neither field 1 or 2 are present for an eye then the grader will not be allowed to access the grading form as the grading will already be considered final.
Focus: Focus refers to the clarity of retinal image. Because of the importance of detecting lesions in the macular area, the grader is to consider focus in 75% or more of the macula area as defined by the 3000μ diameter circle of the Macular Grid. If retinal vessels are sharply defined or slightly fuzzy and small lesions such as retinal microaneurysms and small drusen are visible, the grade is "Good/Fair", code=0. If clarity is decreased so that small retinal lesions might be missed but larger lesions such as geographic atrophy, can be seen, the grade is "Borderline", code=1. If there is a pronounced decrease in sharpness where detail of larger lesions cannot be recognized, the grade is "Poor", code=2. Focus will be graded in both Field 1 and 2.
Photo Quality Problems: Other photo quality problems will be assessed for both images together. If there are other photo quality problems that affect the graders ability to grade the image set, the grader marks "yes" code= 2 and chooses from the following list of problems.
| Code | Definition |
| 0 | No problem |
| 2 | Yes, affects grading |
| 8 | CG photo problems |
Illumination:If an image is poorly illuminated or overexposed, or there are pockets of uneven illumination (a dark macula) then Illumination should be graded "Yes", code=2.
Field Definition: Field 1 is defined a centered on the optic nerve and Field 2 is centered on the macula. If either of these fields deviates more than 1 disc diameter from the optimum location then Field Definition should be graded "Yes", code=2.
Haze - When a green/white halo or partial halo; or a green/white cast throughout the entire photograph is noted, Haze should be graded "Yes", code=2;
Dust - White dots or spots that may be varying size but are in the same location of the image no matter what field of the retina is imaged are usually caused by one or more dirty lenses on the camera. When dust or dirt spots are prominent or located in just the wrong place and cause difficulty in grading, Dust should be graded "Yes", code=2;
Lashes - Lashes or a partial blink often appear on the bottom of the image as either light or dark linear "shadows". These "shadows" can easily obscure the lower half of the image. Occasionally lashes will appear in the upper half of the image as a bright reflectance but dont affect the ability to grade as much. When lashes (or a blink) are present Lashes should be coded "Yes", code =2;
Arc - A small pupil or incorrect patient to camera distance can cause a crescent shaped arc to appear on the image. This arc can range in color from yellow orange to blue and in size from a small slice to an arc that obscures more than half of the field. Arcs normally are found along the nasal or temporal margin rather than the superior or inferior margins although they can occur anywhere. When an Arc is present the grade should be "Yes", code = 2.
Red Channel - A digital image is composed of three color channels, red, green and blue. When the retinas pigmentation is particularly "red" or "light" there can be an overexposure effect where the red channel is saturated or washed out. This will often appear as a pink bleaching between the optic nerve and the macula and can make evaluating retinal lesions in these locations very difficult. When the red channel is washed out the grade should be "Yes", code =2.
Other - if "Other" is noted, describe the quality problem or artifact in the Comment section
Gradability: The grader will judge the overall quality of both images to determine the gradability. If the both fields are focused clearly enough to image the retina, optic nerve and blood vessels without any portion missing or obscured, the image is considered completely gradable. If the more than 75% of optic nerve cannot be graded, but it is possible to grade the macula, the grade is "Disc ungradable", code=1. If a portion of the macula, between 25% (1 DA) and 75 % of the macula cannot be graded, but the optic nerve is gradable, the grade is "Portion macula ungradable", code=2.
If more than 75% of the macula area (diameter=3,000μ, inner circle of Macular Grid) is in poor focus, missing, or obscured by a retinal hemorrhage, vitreous hemorrhage, asteroid hyalosis or some other condition and no lesion of any type is seen but it is possible to grade the disc, the grade is "Macula Ungradable", code=3.
If a portion of the disc and the macula are ungradable (between 25-75% or each) , the grade is code=4. If neither the disc nor the macula can be graded (more than 75% of each), but other portions of the retina are visible, the grade is code=5. If no part of the fields can be graded, the grade is code=6.
If both fields are judged to be ungradable the remaining eye variables will be coded "Cannot Grade" and the grader will complete grading on that eye.
Code | Definition |
0 | All Fields Gradable |
1 | Disc Ungradable |
2 | Portion of Macula Ungradable |
3 | Macula Ungradable |
4 | Portion of Disc and Macula Ungradable |
5 | Disc and Macula Ungradable |
6 | All Fields Ungradable |
3.1.2 Retinal Grading
ARM Exclude : If a condition exists in the macula which confounds the grader from evaluating Age-Related Macular Degeneration (ARM) lesions from similar changes in the retina due to another process the eye should be excluded (cannot grade) from evaluation of all ARM lesions. Typical reasons for excluding an eye are listed below and should be noted in this item. If Other is chosen a Comment should detail the reason for excluding the eye.
| Trauma | Coloboma/ Staphyloma |
| Laser Rx (burns) | Retinopathy of Prematurity (ROP) |
| Vessel Occlusion | Non ARM RPE changes |
| Macular Dystrophy | Non-ARM detachment |
| Myopic Degeneration | Unknown etiology |
| Histoplasmosis/ Toxoplasmosis | Other |
| Inflammatory |
Pathology Notification : If an eye is judged to have a treatable pathologic condition that poses an imminent threat to vision, the Coordinating Center will be notified within three working days of receipt of the images from the site. Notifications will be divided into Immediate (seen by an ophthalmologist ASAP) and Early (seen within 2 months). The reason for pathology notification and the date of notification will be recorded during preliminary grading. If Other is chosen a Comment should detail the reason for pathology notification. Typical pathology notification reasons are listed below:
Reason for Notification? | Type |
Suspicious Cup/Disc (C/D) (>0.7, or 0.7 + notching/undercutting) | Early |
Proliferative Diabetic Retinopathy (level 65+) | Immediate |
Preproliferative Diabetic Retinopathy (level 51) | Early |
Clinically Significant Macular Edema (CSME)? | Immediate |
Edema, not CSME? | Early |
Branch Vein Occlusion (BVO) or Central Vein Occlusion (CVO)? | Early |
Treatable ARM (signs of neovascularization) | Immediate |
Hollenhorst Plaque?? | Immediate |
Irregular Nevus??? | Immediate |
Macular Hole????? | Early |
Epiretinal Membrane with traction in center circle???? | Early |
Other | Either |
ARM Feedback: A preliminary ARM summary variable will be coded to provide timely feedback to the coordinating center for letters to study participant. This variable in no way reflects what the final definition of ARM will be for this eye but is rather a preliminary grade based on clinical definitions rather than research definitions.
No ARM is defined as gradable images with no evidence of lesions associated with ARM.
Drusen Only is defined as at least one soft drusen with a diameter greater than or equal to 125? and a grid area of greater than 500?.
Early ARM is defined as either soft drusen present with a grid area of greater than a 500? circle and a pigmentary abnormality present (increased pigment or depigmentation in the grid) or soft drusen present in the center circle and a pigmentary abnormality is present (increased pigment or depigmentation in the grid).
Late ARM is defined as the presence of any late lesions, such as geographic atrophy, PED/RD detachments, subretinal hemorrhage, subretinal fibrous scar, subretinal new vessels, or laser treatment and/or /photodynamic therapy for ARM.
Cannot Grade ARM is defined as all or some of the ARM lesions are ungradable or confounded by another condition making evaluation of ARM difficult.
The grades for ARM Feedback are:
Code | Definition |
0 | No evidence of age-related macular degeneration |
1 | Drusen only |
2 | Early ARM |
3 | Late ARM |
8 | Cannot Grade ARM |
All other Preliminary Grading variables are defined in the detail grading portion of the protocol. The remaining variables graded during preliminary grading are:
ARM Lesions:
Maximum Drusen Size > 125 micron diameter circle
Soft Drusen (any soft type) Soft Drusen Area > 500 micron diameter circle
Increased Pigment
RPE Depigmentation
Geographic Atrophy
PED/RD Detachment
Subretinal Hemorrhage
Subretinal Fibrous Scar
Laser Rx for ARM
Other Vascular Lesions:
Focal Narrowing
Arterio-venous Crossing Abnormalities
BVO/CVO (branch vein occlusion/central vein occlusion)
BAO/CAO (branch artery occlusion/central artery occlusion)
Hollenhorst Plaque
Other Lesions:
Macular Hole
Large Cup to Disc Ratio (≥ 0.7)
Surface Wrinkling Retinopathy-Traction
Other
Diabetic Retinopathy Level
Macular Edema
3.2 DETAIL GRADING
3.2.1 Image Quality
Field 1 and 2 Presence: If field 1 photograph is present, the grade is "Present", code=2. If the field 1 photograph is absent, the grade is "Absent", code=0. If neither field 1 or 2 are present for an eye then the grader will not be allowed to access the grading form as the grading will already be considered final.
Field 1 and 2 Gradability: The grader will be asked to assess the gradability of both Field 1 and Field 2. If at least one disc area of a field is gradable (good enough focus and illumination to see retinal details) the grader indicates the field is gradable and proceeds with evaluation of the eye. If both fields are judged to be ungradable the remaining eye variables will be coded "Cannot Grade" and the grader will complete grading on that eye.
3.2.2 Retinopathy Sub-section
Retinopathy Level: If there is no evidence of diabetic retinopathy, the grade is code=10, Skip to Item [Other Abnormalities]. If diabetic retinopathy is present, the grader assigns a retinopathy level (see attached Retinopathy Severity Level and Descriptions) and answers all lesion questions. A list of acronyms and their definitions are listed below:
Acronym | Definition |
BVO | branch vein occlusion |
DA | disc area - a standard area of measurement representing the size of the average optic nerve |
DRS | Diabetic Retinopathy Study |
FPD | fibrous proliferation on the disc |
FPE | fibrous proliferation elsewhere |
HE | hard exudates |
HMA | hemorrhages and microaneurysms |
HRC | high risk characteristics for visual loss |
IRMA | intraretinal microvascular abnormality |
MA | microaneurysm |
NPDR | nonproliferative diabetic retinopathy |
NVD | new vessels on the disc |
NVE | new vessels elsewhere |
PDR | proliferative diabetic retinopathy |
PED | pigment epithelial (detachment) |
PRH | preretinal hemorrhage |
Q | questionable |
SE | soft exudates (cottonwool spots) |
SSR | sensory serous retinal (detachment) |
VB | venous beading |
VH | vitreous hemorrhage |
RETINOPATHY SEVERITY LEVEL
LEVEL | DESCRIPTION |
10 | No diabetic retinopathy visible. No other lesions that could be mistaken for diabetic retinopathy. |
11 | Questionable diabetic retinopathy visible. Usually one questionable MA. Especially useful with non-mydriatic or monocular 45? fields as very small MAs may be difficult?????????????????? to discern in these photographs. |
12 | Retinopathy that is non-diabetic in nature, but which could be mistaken for diabetic retinopathy, should be noted in the lesion list (i.e. hard exudate from a SSR/RPE, detachment and HMA and/or IRMA etc. from a BVO). Some of the abnormalities from the global "Other" list would constitute a level 12 in the absence of other diabetic retinopathy. |
14 | Any combination of definite HE, SE, IRMA and/or venous loops in the absence of definite MAs. |
15 | Retinal hemorrhage present without any definite MAs. |
20 | MAs only with no other diabetic lesions present. |
31 | MAs and one or more of the following: HMA < 2A, HE, Venous Loops, Q SE, Q IRMA, Q VB. |
41 | MAs and one or more of the following: SE, IRMA < 8A. |
51 | MAs and one or more of the following: VB, HMA = 2A, IRMA = 8A. |
60 | FP only with no other proliferative lesions. |
61 | No retinopathy and scatter treatment (rx) scars present |
62 | Level 20 (MAs only) and scatter treatment (rx) scars present |
63 | Level 31 (Early NPDR) and scatter treatment (rx) scars present |
64 | Levels 41 or 51 (Moderate or Severe NPDR) and scatter treatment (rx) scars present |
65 | PDR < HRC. Any proliferative lesions that do not constitute DRS high risk characteristics. |
70 | PDR = HRC: NVD = 10A |
80 | Total VH. Cannot grade the fundus through the VH haze. This can be verified with a dark or black-red reflex picture |
88 | Cannot assign an accurate retinopathy level usually due to poor photo quality. While the level may be 88, some lesions may be gradable |
All diabetic lesions HMA, HE, SE, IRMA, VB, NVD, NVE, FP, and PRH/VH are graded according to the ETDRS protocol.
Macular Edema (ME): Increased permeability of retinal capillaries and retinal microaneurysms may result in an accumulation of extracellular fluid and thickening of the normally compact retinal tissue. Initially, there may be a slight loss of the normal transparency of the retina and the edema may be missed easily. The leakage and resulting edema may be focal around retinal microaneurysms or be diffuse and in some cases lead to the appearance of cystoid spaces in the outer retina. In the absence of stereo the grader will look for signs of leakage, such as rings of organized hard exudate, localized areas of color change and a deviation of the normal pathway of the retinal blood vessels. Clinically significant macular edema (CSME) is considered present when edema involves the fovea or is within 500 microns of the fovea, or when a 1+ disc area of edema is present with at least a portion of it within the macula.
Code | Definition |
0 | No Macular Edema (ME) is present. |
1 | Questionable ME |
2 | Definite ME but not Clinically Significant (CSME) |
3 | CSME is present |
7 | Edema is present but not diabetic |
8 | Cannot grade. |
Macular Edema-Central Circle (CC): The grader assesses edema in the center circle. The choices are:
Code | Definition |
0 | No ME in the center circle |
1 | Questionable ME in the center circle |
2 | Definite, CSME, but no cysts |
3 | CSME with cysts |
7 | Edema is present but not diabetic |
8 | Cannot grade center circle |
Photocoagulation (PC) Scar: Local and/or scatter photocoagulation (panretinal or PRP) treatment is usually done to treat neovascularization (also retinal detachment) as a result of diabetes. (also used for retinal vein occlusion or a retinal tear.)
Code | Definition |
0 | No photocoagulation scars are present |
1 | Questionable or incomplete photocoagulation scars are present |
2 | Local photocoagulation scars only are present |
3 | Scatter photocoagulation scars only are present |
4 | Scatter + Local photocoagulation scars are present |
8 | Cannot grade for photocoagulation scars |
Focal Photocoagulation (PC) Treatment : Focal laser photocoagulation, either as treatment of leaking retinal microaneurysms (MAs) or in a grid pattern, is done for the treatment of localized (MA Rx) or diffuse macular edema (grid Rx). If focal treatment cannot be assessed the grade is code 8.
Code | Definition |
0 | No focal burns present |
1 | Questionable focal burns present |
2 | Focal MA burns only |
3 | Grid pattern of burns only |
4 | Focal + grid burns are present |
8 | Cannot grade focal burns |
3.2.3 Arteriolar Abnormalities
The arteriolar abnormalities assessed are: focal narrowing and arterio-venous crossing abnormalities (arterio-venous nicking). All abnormalities are assessed outside of Zone A on the Optic Nerve Grid.
Focal Retinal Arteriolar Narrowing in Quadrants
The grader assesses all marked constrictions of retinal arteries and arterioles in Field 1 outside of Zone A as focal narrowing. (The overlapping portions of Field 2 may be used to confirm the presence of focal narrowing in Field 1.) Definite focal narrowing in Field 1 is graded when the involved vessel is at least 40μ in diameter, or about 1/3 of the diameter of a vein at the disc margin, and the constricted area has a caliber less than or equal to 1/2 the caliber of proximal and distal vessel segments. The focal "pinch" must be at least 250μ in length to be considered definite. If the grader observes constriction in vessels less than 40μ in diameter, such constrictions should be assessed as questionable focal narrowing. If the grader feels that subtle constriction of vessels is present or that a definite "pinch" is present but the length is shorter than 250μ long, the grader marks questionable focal narrowing.
Focal narrowing or constriction of retinal arterioles is assessed in each of the four quadrants, excluding the area within 1/2 DD of the disc (Zone A). The photograph grader places the Optic Nerve Grid on the Field 1 image and carefully examines all arterioles greater than or equal to 40μ in diameter, or about 1/3 the diameter of a vein at the disc margin, and evaluates the arteriole for constricted segments. There is sometimes a gradual tapering from the original caliber of the arteriole to the most constricted caliber; only the length of constriction to 1/2 or less of the original caliber is considered definite. If focal narrowing extends from one quadrant to another, the narrowing is estimated separately in each quadrant. If the total length of arterioles available for examination in a quadrant totals less than 1 1/2 DD, then the grader marks that quadrant ungradable, code 8. Cannot grade is also used if the arterioles in a given subfield are out-of-focus or obscured by artifact.
Each quadrant, superior temporal (ST), superior nasal (SN), inferior temporal (IT) and inferior nasal (IN) is evaluated for the absence of presence of focal narrowing. The following codes are used:
Code | Definition |
0 | No focal narrowing. |
1 | Questionable focal narrowing. |
2 | Definite focal narrowing |
8 | Cannot grade. |
Arterio-Venous Nicking in Quadrants
The photograph grader assesses abnormalities of arterio-venous crossings, or arteriovenous nicking (AV nicking), in each quadrant. Both Field 1 and 2 are used for this evaluation with the grader mentally extending the temporal quadrants through Field 2. Crossings within 1/2 DD of the disc margins (Zone A) are excluded, as are the atypical crossings where the vein crosses over the artery. The grader examines all crossings of artery over vein, and evaluates crossings where the venous blood column is narrowed as abnormal.
Tapering or narrowing of the venous blood column on three or all four sides of the crossing is required for definite AV. If the venous blood column appears tapered on only two sides of the crossing, and the appearance is not due to normal vessel undulation, then the grader assesses AV nicking as questionable. If only one side of the venous column is "nicked" the grader considers A/V nicking absent. The grader discounts any apparent diminishments in venous caliber if the vein appears to be partially obscured by nerve fiber reflex as it approaches and crosses under the artery.
Each quadrant, superior temporal (ST), superior nasal (SN), inferior temporal (IT) and inferior nasal (IN) is evaluated for the absence of presence of AV nicking. The following codes are used:
Code | Definition |
0 | No AV nicking. |
1 | Questionable AV nicking. |
2 | Definite AV nicking. |
8 | Cannot grade. |
Example photograph A6 exhibits one definite arterio-venous crossing abnormality in the superior temporal (ST) quadrant. Subtle tapering of the venous blood column can be seen on both sides of the crossing, and the Z-shaped deviation in the path of the vein further suggests that the pressure relationships at the crossing are not normal. The arterio-venous crossing in the inferior temporal (IT) quadrant is similar in appearance but the tapering of the venous blood column cannot be seen distinctly on the proximal side of the crossing; therefore, the IT quadrant would be marked questionable for arterio-venous crossing abnormalities.
The arterio-venous crossing abnormalities in example photograph Example photograph A7 are more pronounced. Both the inferior nasal (IN) and superior temporal (ST) quadrants exhibit marked narrowing of the venous caliber on both sides of the arterio-venous crossing in question. In the ST quadrant, the caliber of the vein narrows to about 1/3 of its normal caliber, resulting in a grade of severe. The inferior temporal (IT) quadrant has an arteriovenous crossing immediately adjacent to a venous trifurcation. The venous branch involved in the this crossing is visibly narrowed distally, but the proximal side cannot be assessed because of the proximity to the trifurcation. Because the venous narrowing is visible on only one side, arterio-venous nicking would be assessed as questionable in the IT quadrant.
Example photograph A8 exhibits definite, although somewhat more subtle, arteriovenous nicking in both temporal quadrants. The abnormal arterio-venous crossing in the IT quadrant is adjacent to a venous bifurcation. In this case, the crossing is somewhat distal to the bifurcation and the venous caliber can be assessed on both sides of the crossing. The venous caliber on both sides is narrower than the caliber of the vein distally in the field. The ST quadrant shows narrowing of the vein on both sides of the crossing, although the narrowing on the proximal side is more subtle than that seen in the other examples.
3.2.4 Other Vascular Changes
The grader is asked to evaluate the absence or presence of other vascular abnormalities in the retina. The following list of abnormalities are evaluated and graded using these codes:
Code | Definition |
0 | None present. |
1 | Questionably present. |
2 | Definitely present but not in the center circle |
3 | Definitely present and the center circle is involved. |
8 | Cannot grade. |
Branch Vein Occlusion- Obstruction of a branch retinal venule. An older occlusion may demonstrate sheathed venules and retinal collateral vessels. Localized hemorrhages and/or IRMAs are commonly present. The occluded vessel may not always be obvious.
Central Vein Occlusion- Obstruction of a central retinal venule. A fresh occlusion is distinguished by dilated retinal venules and diffuse retinal hemorrhages.
Branch/Central Artery Occlusion- Obstruction of a branch or central retinal arteriole. If "fresh", may be associated with large grayish-white area of retinal infarction. Either generalized or localized ischemia may be noted.
Hollenhorst Plaque- Cholesterol emboli. These highly-refractile to smudgy-white lesions lie within arterioles and are quite often seen at artery bifurcations. Care must be taken to distinguish from old retinal macroaneurysms or underlying drusen. (Code 3, center circle, is not applicable.)
3.2.5 Age-related Maculopathy (variable =ANY ARM)
The following lesions are graded using the same codes as the Other Vascular Changes list that is detailed above. ARM lesions are only to be evaluated in the macular grid area in Field 2. If soft drusen or other ARM-like lesions are present outside the grid they should be coded under Any Other/ Other and detailed in the comments.
Maximum Drusen Size > 125 micron diameter circle - Drusen are described as round or ovate, sometimes slightly elevated deposits of variable size, usually located in the plane of the retinal pigment epithelium (RPE). Drusen are classified according to diameter. It is assumed that all drusen are round or oval in shape and that a single druse is no more than twice as long as it is wide. If a druse is oval, its shorter diameter is used to classify its size. Standard circles C-0 (63 micron diameter), C-1 (125 micron diameter) and/or C-2 (250 micron diameter) are superimposed over or placed next to the largest druse in the grid area. If the shorter diameter of the druse equals or exceeds the diameter of the circle, the druse is judged to be equal to or greater than this circle in size. In using the circles, judge from the center of the line. If any portion of a drusen judged to be >
125 microns in diameter (C1) is contained inside the grid then the grade is "Yes", code =2.
Soft Distinct Drusen- These drusen are usually larger in size then hard distinct drusen (between 63 and 300 microns in diameter). Soft distinct drusen have sharp margins and a round nodular appearance with a uniform density (color) from center to periphery.
Soft Indistinct (or Reticular) Drusen- Soft indistinct drusen are the same size as the soft distinct but have indistinct margins and a softer, less solid appearance. These druse appear to be disintegrating around the edges and quite often have uneven coloring and thickness within. Reticular drusen appear to be Soft Indistinct Drusen arranged into ill-defined networks of broad interlacing ribbons. They form a grid pattern with very subtle borders.
Soft Drusen Area - The area involved with soft drusen is measured using the appropriate grid. If the area of soft drusen within the center circle is greater than a 500 micron diameter circle than code 3 (Yes, Center Circle) is selected. Otherwise, if the area is greater than a 500 micron diameter circle (not in the center circle) within the entire grid area than code 2 (Yes) is selected. If soft drusen is present but the area is less than a 500 micron circle than code 0, No is selected. (Questionable is not an allowed answer for this item.)
Increased Pigment (Hyperpigmentation) - Age-related deposition of granules or clumps of grey or black pigment in or beneath the retina. When increased pigmentation is present outside of the macular area or is considered due to another cause, "Other" is marked and a comment included.
RPE Depigmentation (RPE degeneration) - Age-related depigmentation of retinal pigment epithelium characterized by faint grayish-yellow or pinkish-yellow areas of varying density and configuration without sharply defined borders. Increased pigment is frequently seen over and adjacent to these areas. When RPE degeneration is judged to definitely not be a result of ARM, Any Other "Other" should be marked and a comment included.
Geographic Atrophy - Appears as a sharply defined area of drop-out of retinal pigment epithelium and choriocapillaries, exposing choroidal vessels as a result of degeneration of the deep layers of the retina. When atrophic lesions are definitely not a result of ARM, Any Other "Other" should be marked and a comment included.
PED/Retinal Detachment (SSR Detachment) - Clear or solid dome-shaped fluidfilled elevation indicating a serous or retinal pigment epithelium detachment of the retina. In the absence of stereo the grader will look for lines of demarcation, color change and vessel deviation in the macula as cues. The presence of other early or late ARM lesions in the vicinity of these changes will help to confirm a detachment is present. When PED/RD is definitely not a result of ARM, "Other" should be marked and a comment included.
Sub-retinal Hemorrhage - Hemorrhage below the retinal surface which may appear as a dark red, dark grey or greenish area. When sub-retinal hemorrhage is definitely not a result of ARM, "Other" should be marked and a comment included.
Sub-Retinal New Vessels (SRNV) - Abnormal blood vessels that grow beneath the RPE/retina. They will often appear as a dilated choroidal like vessel adjacent to a detachment, or subretinal scar or hemorrhage. These blood vessels are difficult to detect in a color fundus image without the aid of an angiogram, but occasionally they can be seen.
Sub-retinal Fibrous Scar (Disciform Scar) - Sheets or mounds of "white" material appearing like a scar, involving the retina. When sub-retinal fibrous scarring is definitely not a result of ARM, "Other" should be marked and a comment included.
Photocoagulation Treatment for ARM- Localized treatment within the arcades for subretinal new vessels due to ARM. This often appears as a deep and heavy white scar. Photodynamic therapy, a light activated chemical, which "clots" in neovascular membranes should be included in this category.
3.2.6 Other Abnormalities:
The following lesions are graded using same codes as the Other Vascular Changes list that is detailed above.
Peripapillary Atrophy - Choroidal atrophic area around disc, usually ≥ 1/2 the circumference of the disc and definitely not considered scleral crescents. If the atrophic area is on temporal side of the disc and fairly symmetric, it is usually a myopic or scleral crescent and should not be marked as peripapillary atrophy. (Code 3, center circle, is not applicable.)
Macular Hole - Round or sharply defined hole in the center of the macula. May be surrounded by a gray halo of detachment of the retina. Thinning and depigmentation of the RPE develop within the hole and small retinal cysts may be evident near the hole.
Large Cup-to-Disc Ratio - If the cup-to-disc ratio is equal to 0.6, "Q" is marked and the ratio is noted in Comments. If the cup-to-disc ratio is >0.6, "Yes" is chosen and the cup-to-disc ratio is noted in Comments. (Code 3, center circle, is not applicable.)
Asteroid Hyalosis- Multiple spherical and stellate opacities in the vitreous. May be difficult to differentiate in non-stereoscopic photographs. Should appear in front of vessels and disc. Care must be taken to differentiate from retinal drusen. If asteroid hyalosis is dense, may prevent grading drusen.
Nevus - Localized increase in number of pigment bearing cells of the choroid, usually in a round or oval shape. Lack of stereopsis will make it difficult to differentiate from raised lesion (melanoma). May have drusen overlying the lesion. If possible, should be distinguished from "bear tracks" and other hyperpigmentation of the retinal pigment epithelium.
Surface Wrinkling Retinopathy -Traction - (SWR-Traction) Slight contraction of the thin membrane on the inner surface of retina. Can be associated with patches of cellophane reflex (see below). If only cellophane reflex is present, SWRTraction should be not be coded, instead SWR -Cello should be coded as present.
Surface Wrinkling Retinopathy - Cellophane Reflex - (SWR-Cello) A patch or patches of irregular increased reflection from the inner surface of retina (cellophane reflex) which may be associated with fine traction lines and vascular tortuosity. If only traction lines are present , SWR-Cello should not be coded, only SWR-Traction should be coded as present.
Histoplasmosis (POHS) - Presumed Ocular Histoplasmosis Syndrome (POHS) is characterized by one or more of the following: multiple peripheral atrophic chorioretinal scars, peripapillary chorioretinal scarring, and/or macular subretinal fibrous scar. If the latter is present without other signs of POHS, code only Subretinal Fibrous Scar as code=2.
Retinal Detachment - A condition in which the inner layers of the retina are pulled/separated from the pigment layer.
Photocoagulation Treatment for other conditions (Rx Other)- Miscellaneous treatment for other conditions such as branch vein occlusions or retinal detachment.
Chorioretinal Abnormalities/Other- Retinal and/or choroidal degeneration, regardless of cause, which does not appear to be associated with age-related maculopathy.
Other - Detail in the Comment section.
Comments: A comment is necessary if:
- Photo Quality Problem, "Other" is chosen;
- ARM Exclude, "Other" is chosen;
- Pathology Notification, "Other" is chosen;
- Any Other, "Other" is chosen;
- A comment may be noted for any other unusual feature found.
4. Grading System
The grading system includes a preliminary and detailed grading followed by a photograph edit and adjudication if necessary. Each set of images will be graded on the items detailed above using custom designed computer software with built in completeness and consistency checks. Upon completion of this detailed grading, a comparison will be made between the preliminary grading and the detailed grading. If there is a disagreement in the levels assigned for specific lesions, the eye will be sent to a third grader for an edited grade of those lesions. If the edited grade still does not agree with either the preliminary or detailed score, then the eye will be sent to the consulting ophthalmologist for adjudication.
Note: Example photographs A6, A7, and A8 referenced in the digital grading section of this protocol are provided and used with permission by the Atherosclerosis Risk in Communities (ARIC) Study Research Group.
Personnel and Training Required
Before attempting photography, the photographer should become very familiar with the camera through a training session and by learning the terminology on pages 4 and 5 of the Canon Non-Mydriatic Retinal Camera CR6-45NM Operation Manual. This Retinal Photography Protocol uses terminology from the Operation Manual and it is recommended that the entire manual be reviewed by each photographer before performing photography.
PHOTOGRAPHER CERTIFICATION
Certification of Photographers
Each examiner taking fundus photographs will need to become certified before taking photographs for the study. A certified photographer will provide complete instruction and copies of the Ocular Epidemiology Photography Protocol and Canon Non-Mydriatic Retinal Camera CR6-45NM Operation Manual. The trainee photographer will practice on volunteers and, when ready, prepare and submit photographs of 10 eyes (5 right eyes and 5 left eyes) photographed following the study protocol for consideration for certification. A photographer is fully certified after submitting satisfactory quality photographs of 10 eyes taken on non-study volunteers. These photographs must show proper field definition (Fields 1 and 2 of each eye, 20 images total), proper exposure, alignment and focus.
Certification Maintenance Requirements
In order to maintain certification, photographers must complete photograph a minimum of six eyes per month and 75% of their photographs must be gradable. This will be determined from the monthly photo quality report generated by the study coordinator. If a photographer fails to meet either of these requirements, he or she will be contacted and given feedback by a photography consultant. During the following month, the photographer will be allowed to continue to take photographs of study participants only if supervised by a fully compliant certified photographer. If the photographer does not meet these standards of quantity or quality of their photographs for three consecutive months, certification will be revoked. The technician will not be able to take study photographs until he/she has submitted a new set of acceptable certification photographs.
Equipment Needs
Equipment for capturing digital images:
A Canon CR6-45NM fundus camera equipped with a digital Canon D-60 camera back will be used. A laptop computer, supported by an articulating arm, will contain image acquisition and archive software EyeQSL, provided by Digital Healthcare Inc. The fundus camera and computer are mounted on a motorized instrument table to allow maximum subject comfort and optimum camera alignment. Both photographer and subjects have pneumatically adjustable stools with a backrest.
Other Supplies:
(a) Lens cotton (long-grain Red Cross sterile cotton batting)
(b) Lens cleaning alcohol (100% alcohol)
(c) Facial tissues
(d) Spare view lamp (#BH3-3277)
(e) Canon camera fuses (125V, 4 amp)
(f) CDs and jewel cases
Equipment for reviewing digital images:
The photograph grader views each retinal image with a high resolution monitor using the EyeQ Lite image processing software and database, and references the written protocol and the digital photographic standards and examples to evaluate retinal abnormalities. The photograph grader directly enters his/her evaluations in a micro computer database. The following materials are used in the reading process:
(a) Minimum Intel based 900 Mghz PC running Windows 2000 or XP with 256 MB of RAM and a dual monitor capable graphics card (recommended ATI Radeon All-in-Wonder card);
(b) Primary monitor, 21 inch for image viewing, set to a resolution of 1600 X 1200 with 32 bit color, standardized using Verilum calibration software;
(c) Secondary monitor, recommended minimum 15 inch LCD, set to 1024 X 768 resolution (actual value not as critical as this monitor will display the data collection database);
(d) Digital Healthcare EyeQ Lite or Pro image processing software version 4.8 or higher;
(e) MESA-EYE ACCESS database, a direct entry software with a series of data collection screens built in ACCESS available to graders on networked personal computers, and based on the paper data collection form.
This protocol uses the Canon Non-Mydriatic Retinal CR6-45NM camera with a digital Canon D60 camera back (6.3 megapixels per image). Other ophthalmic imaging cameras can be used. If other instruments are used, the reproducibility of the measurements should be comparable to those acquired with this protocol. The Ocular Working Group recommends cameras that capture images that are 5 mega-pixels or larger for use in grading and vessel measurement protocols. When other instruments are used to capture digital retinal images, the manufacturer and model of equipment should be recorded. These other cameras may require some different steps than are described in this protocol. Investigators should follow the equipment manufacturers instructions to ensure quality control.
In addition, this protocol uses EyeQSL,software which is commercially available through Digital Healthcare Inc. The Ocular Working Group notes that other ophthalmic imaging packages are available through other vendors that are similar in nature. These other software packages may require some different steps than are described in this protocol. Investigators should follow the manufactures instructions to ensure quality control. Please be sure to record the manufacturer and model and version of the software used.
Requirements
| Requirement Category | Required |
|---|---|
| Major equipment | Yes |
| Specialized training | Yes |
| Specialized requirements for biospecimen collection | No |
| Average time of greater than 15 minutes in an unaffected individual | No |
Mode of Administration
Clinical Measurement
Lifestage
Child, Adolescent, Adult
Participants
Adults aged 45 to 84 years*
*While this protocol was used in a study of adults aged 45 to 84 years, the Ocular Working Groups suggests that the same methodology can be used for individuals below age 45 and for children who are old enough to be able to tolerate the exam (usually by age 5).
Selection Rationale
Retinal imaging is useful for any study where information on specific conditions affecting the retina or retinal vascular caliber is important. Retinal vascular caliber (both venular and arteriolar) has been associated with macrovascular disease such as stroke, coronary heart disease and hypertension, and diabetes.
Language
Chinese, English
Standards
| Standard | Name | ID | Source |
|---|---|---|---|
| Logical Observation Identifiers Names and Codes (LOINC) | Retinal digital photography proto | 62709-1 | LOINC |
| Human Phenotype Ontology | Abnormality of the eye | HP:0000478 | HPO |
| caDSR Form | PhenX PX111501 - Retinal Digital Photography | 5973778 | caDSR Form |
Derived Variables
None
Process and Review
Not applicable.
Protocol Name from Source
National Heart, Lung and Blood Institute (NHLBI), Multi-Ethnic Study of Atherosclerosis (MESA), 2000-2008
Source
National Heart, Lung and Blood Institute, Multi-Ethnic Study of Atherosclerosis (MESA), 2000-2008MESA-Eye Photography Protocol
MESA-Eye Digital Grading Protocol (12/08/05)
General References
Klein R, Klein BE, Knudtson MD, Wong TY, Cotch MF, Liu K, Burke G, Saad MF, Jacobs DR Jr. (2006). Prevalence of age-related macular degeneration in 4 racial/ethnic groups in the multi-ethnic study of atherosclerosis. Ophthalmology, 113(3)373-380.
Wong TY, Islam FM, Klein R, Klein BE, Cotch MF, Castro C, Sharrett AR, Shahar E. (2006). Retinal vascular caliber, cardiovascular risk factors, and inflammation: the multi-ethnic study of atherosclerosis (MESA). Invest Ophthalmol Vis Sci, 47(6)2341-2350.
Cheung N, Bluemke DA, Klein R, Sharrett AR, Islam FM, Cotch MF, Klein BE, Criqui MH, Wong TY.(2007). Retinal arteriolar narrowing and left ventricular remodeling: the multi-ethnic study of atherosclerosis. J Am Coll Cardiol, 50(1)48-55.
Cheung N, Sharrett AR, Klein R, Criqui MH, Islam FM, Macura KJ, Cotch MF, Klein BE, Wong TY. (2007). Aortic distensibility and retinal arteriolar narrowing: the Multi-Ethnic Study of Atherosclerosis. Hypertension, 50(4)617-622.
Cheung N, Klein R, Wang JJ, Cotch MF, Islam AF, Klein BE, Cushman M, Wong TY. (2008). Traditional and novel cardiovascular risk factors for retinal vein occlusion: the multiethnic study of atherosclerosis. Invest Ophthalmol Vis Sci, 49(10):4297-302.
Kawasaki R, Cheung N, Wang JJ, Klein R, Klein BE, Cotch MF, Sharrett AR, Shea S, Islam FA, Wong TY. (2009). Retinal vessel diameters and risk of hypertension: the Multiethnic Study of Atherosclerosis. J Hypertens, 27(12):2386-93.
Protocol ID
111501
Variables
Export Variables| Variable Name | Variable ID | Variable Description | dbGaP Mapping | |
|---|---|---|---|---|
| PX111501_Left_Eye_Estimated_Pupil_Diameter | ||||
| PX111501120000 | Left Eye Estimated Diameter of Pupil at 1st more | N/A | ||
| PX111501_Left_Eye_Number_Images_Captured | ||||
| PX111501110000 | Left Eye Number of images captured in the more | N/A | ||
| PX111501_Left_Eye_Problem | ||||
| PX111501130000 | Left Eye Describe any problems or unusual findings | N/A | ||
| PX111501_Left_Eye_RDG_Fields_Cannot_Be_Photographed | ||||
| PX111501090100 | Left Eye Fields cannot be photographed in more | Variable Mapping | ||
| PX111501_Left_Eye_RDG_Fields_Other | ||||
| PX111501090200 | Left Eye Fields photographed in the Retinal more | N/A | ||
| PX111501_Left_Eye_RDG_Fields_Photographed | ||||
| PX111501090000 | Left Eye Fields photographed in the Retinal more | N/A | ||
| PX111501_Left_Eye_RDG_Flash_Setting | ||||
| PX111501100000 | Left Eye Flash Setting in the Retinal more | N/A | ||
| PX111501_Participant_ID | ||||
| PX111501010000 | Participant ID | Variable Mapping | ||
| PX111501_Photographer_ID | ||||
| PX111501020000 | Photographer ID | N/A | ||
| PX111501_Retinal_Digital_Photography_Instrument_Model | ||||
| PX111501030000 | Retinal Digital Photography instrument model | N/A | ||
| PX111501_Right_Eye_Estimated_Pupil_Diameter | ||||
| PX111501070000 | Right Eye Estimated Diameter of Pupil at 1st more | N/A | ||
| PX111501_Right_Eye_Number_Images_Captured | ||||
| PX111501060000 | Right Eye Number of images captured in the more | N/A | ||
| PX111501_Right_Eye_Problem | ||||
| PX111501080000 | Right Eye Describe any problems or unusual more | N/A | ||
| PX111501_Right_Eye_RDG_Fields_Cannot_Be_Photographed | ||||
| PX111501040100 | Right Eye Fields cannot be photographed in more | Variable Mapping | ||
| PX111501_Right_Eye_RDG_Fields_Other | ||||
| PX111501040200 | Right Eye Fields photographed in the Retinal more | N/A | ||
| PX111501_Right_Eye_RDG_Fields_Photographed | ||||
| PX111501040000 | Right Eye Fields photographed in the Retinal more | N/A | ||
| PX111501_Right_Eye_RDG_Flash_Setting | ||||
| PX111501050000 | Right Eye Flash Setting in the Retinal more | N/A | ||
Measure Name
Retinal Digital Photography
Release Date
February 26, 2010
Definition
A method to photograph (image) the retina, optic disc, macula, and posterior pole (i.e. the fundus) using a specialized lens system with a digital camera back.
Purpose
These images are necessary to document the status of the retina, optic nerve, retinal blood vessels, and macula. The photographs are used for documentation and for comparison from year to year for a subject and between subjects. Various eye diseases can be imaged with digital photography such as diabetic retinopathy, glaucoma, macular degeneration, retinal detachment, hypertensive retinopathy, holes in the retina, as well as many other acquired and congenital eye conditions.
Keywords
Ocular, Eye, Retinal image, Multi-Ethnic Study of Atherosclerosis, MESA
Measure Protocols
| Protocol ID | Protocol Name |
|---|---|
| 111501 | Retinal Digital Photography |