Protocol - Waist Circumference - Waist Circumference NHANES
- Body Composition - Body Composition by Dual-Energy X-Ray Absorptiometry
- Body Composition - Subscapular Skinfold Thickness
- Body Composition - Suprailiac Skinfold Thickness
- Body Composition - Triceps Skinfold Thickness
- Ethnicity and Race
- Growth Charts
- Height - Knee Height
- Height - Recumbent Length
- Height - Self-Reported Height
- Height - Standing Height
- Hip Circumference - Hip Circumference
- Maximum Adult Weight
- Weight - Measured Weight
- Weight - Self-Reported Weight
- Weight Loss/Gain
Description
Waist circumference is measured at several body sites in the scientific literature. For the National Health and Nutrition Examination Survey (NHANES), the measurement of the participant’s abdominal (waist) circumference is made at the uppermost lateral border of the ilium using a tape measure. This measurement protocol was developed specifically for NHANES III (1988-1994) to improve reliability by standardizing the bony landmarks needed to determine the plane for measurement, and it is rarely used outside of the United States. In both children and adults, and compared with measurements taken using other protocols, measurements taken over the iliac crest tend to be several centimeters larger than measurements taken midway between the lowest rib and iliac crest (Waist Circumference - Waist Circumference NCFS) or at the level of the umbilicus (Waist Circumference - Framingham Heart Study), except when waist circumference is measured at the level of the umbilicus in an obese participant and the umbilicus has been displaced downward (i.e., pendulous abdomen). This protocol is recommended for use by the National Heart, Lung, and Blood Institute to define central obesity (greater than 102 cm in men; greater than 88 cm in women), and references by race/ethnicity have been developed for children and adolescents. It should not be used to calculate a waist-to-height ratio (WHtR) because it will overestimate the prevalence in the abnormal range (WHtR greater than 0.5). The relationship of this measure with cardiometabolic risk factors is, however, comparable with waist circumference measures taken at other sites.
NOTE: Waist circumference can be measured on pregnant women. However, national reference data do not include pregnant women, and waist circumference has different associations with abdominal and total body fat among those who are not pregnant.
Specific Instructions
Several overarching, critical issues for high-quality data collection of anthropometric measures that optimize the data in gene-environment etiologic research include (1) the need for training (and retraining) of study staff in anthropometric data collection; (2) duplicate collection of measurements, especially under field conditions; (3) use of more than one person for proper collection of measurements where required; (4) accurate recording of the protocols and measurement units of data collection; and (5) use of required and properly calibrated equipment.
The notion of recommending replicate measurements comes from the reduction in random errors of measurement and accompanying improved measurement reliability when the mean of multiple measurements is used rather than a single measurement. This improvement in measurement reliability, however, depends on the reliability of a single measurement in the hands of the data collectors in a particular study (Himes, 1989). For example, if a measure such as recumbent length in a given study has a measurement reliability of 0.95 (expressed as an intraclass correlation coefficient), taking a second measurement and using the mean of the two measurements in analyses will improve the reliability to only 0.97, yielding only a 2% reduction in error variance for the additional effort. If, in the same study, the reliability of a single triceps skinfold measurement was 0.85, using the mean, including a replicate measurement, would raise the reliability to 0.92 and yield a 7% reduction in error variance, more than a three-fold improvement compared with recumbent length. The intraclass correlation coefficient is specifically recommended here for assessing reliability because it takes account of both random and systematic errors of measurement, whereas the interclass correlation (e.g., Pearson correlation) takes account of only random errors of measurement.
Because the benefits of taking replicate measurements are so closely linked with the existing measurement reliability, it is recommended that as a part of the training of those who will be collecting anthropometry data, a reliability study be conducted that will yield measurement reliability estimates for the data collectors, protocols, settings, and participants involved in that particular study (Himes, 1989). If the measurement reliability for a single measurement is greater than or equal to 0.95, the recommendation is that replicate measurements are not necessary and will yield little practical benefit. If the measurement reliability is less than 0.95, the recommendation is to include replicate measurements as prescribed.
If replicate measurements are indicated because of relatively low reliability, a second measurement should be taken, including repositioning the participant. A third measurement should be taken if the first two measurements differ by more than 1.0 cm in those 12 years or older and by more than 0.50 cm in those younger than 12 years. If it is necessary to take a third measurement, the two closest measurements are averaged. Should the third measurement fall equally between the first two measurements, all three should be averaged.
Note: Detailed videos illustrating the procedure can be found here: https://www.youtube.com/watch?v=myaB4eZDBBc
The state of the science does not indicate a clear choice of protocol at this time. Therefore, the PhenX Expert Review Panel recommends that one protocol be selected in measuring the waist circumference and that the protocol correspond to the reference data used. Further, the exact protocol used should be recorded and reported.
These recommendations differ from those included in the original PhenX datasheets. Previously, slightly different protocols were recommended for youth and adults; these are now combined into three protocols appropriate for all age groups. Also, it is now recommended that only one protocol be used in a particular study rather than using all three protocols.
Availability
This protocol is freely available; permission not required for use.
Protocol
Abdominal (Waist) Circumference
Exam staff will collect the waist circumference on participants aged 2 years and older. Follow the procedures below to obtain this measure:
1. Position the SP. Instruct the SP to gather the shirt gown above the waist and clip it on the front so it will not interfere with the measurements. Instruct the participant to cross his or her arms and place his or her hands on opposite shoulders. Demonstrate the desired position of the arms. It may help to tell SPs to think of giving themselves a hug.
Feel the SP’s right and left iliac crest and, if necessary, lower the waistband of the pants and underclothing to expose the iliac crest. Again, always tell the SP what you are going to do before you do it.
2. Mark the Measurement Site. Stand on the participant’s right side. Palpate the hip area to locate the right ilium of the pelvis. With the cosmetic pencil draw a horizontal line just above the uppermost lateral border of the right ilium. Cross this mark at the midaxillary line, which extends from the armpit down the side of the torso.
Note: If it is difficult to find the iliac crest, such as on SPs with larger waists, then begin inferior to the midaxillary line (toward the SP’s front) and palpate the ilium upward to the midaxillary line until you find the uppermost part of the bone. Exhibit 1 shows the measurement site correctly marked for the waist circumference.
3. Take the Measurement. Extend the measuring tape around the waist. Position the tape in a horizontal plane at the level of the measurement mark (Exhibit 2). Use the wall mirror to ensure the horizontal alignment of the tape. While the examiner remains on the SP’s right side, the recorder will come around to the SP’s left side to check the placement of the tape. Check that the tape sits parallel to the floor and lies snug but does not compress the skin. Always position the zero end of the tape below the section containing the measurement value. Take the measurement to the nearest 0.1 cm at the end of the SP’s normal expiration.
4. Record the Result. Call the result to the recorder, who will enter this number on the ISIS screen. Remove the tape measure and erase the cosmetic pencil mark from the SP’s skin with a few drops of baby oil on a piece of gauze.
Exhibit 1. Waist circumference mark
 |  |
Exhibit 2. Measuring tape position for waist circumference
 |  |
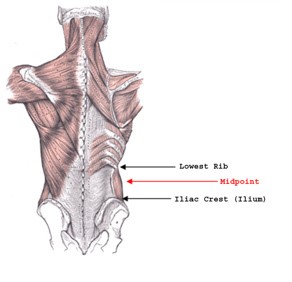
Note: Graphic from the "For Good Measure" Study. Personal Communication, M. Forman. Exhibit 3 displays the anatomical features that are referenced by the various PhenX waist circumference measurement protocols (see Waist Circumference - Waist Circumference NCFS and Waist Circumference - Framingham Heart Study).
Exhibit 3. Location of Measurement Landmarks between the Lowest Rib and Iliac Crest (Ilium).
Personnel and Training Required
None
Equipment Needs
None
Requirements
| Requirement Category | Required |
|---|---|
| Major equipment | No |
| Specialized training | No |
| Specialized requirements for biospecimen collection | No |
| Average time of greater than 15 minutes in an unaffected individual | No |
Mode of Administration
Physical Examination
Lifestage
Infant, Toddler, Child, Adolescent, Adult, Senior
Participants
Participant aged 16 years or older, although the protocol can be used at ages 2 years or older
Selection Rationale
The National Health and Nutrition Examination Survey 2021-2023 protocols were selected as best practice methodology and are the most widely used protocols to assess Abdominal (Waist) Circumference at the iliac crest.
Language
Chinese, English, Spanish
While the English version of this protocol has been updated, the available translations have not and reflect a previous version. These differences may impact the compatibility between the English and Spanish/Chinese versions. It is the responsibility of the investigator to determine if the translations are sufficiently compatible with the English version for their research and subsequent analysis.
Standards
| Standard | Name | ID | Source |
|---|---|---|---|
| caDSR Form | Px21604 Waist Circumference Waist Circumference Nhanes | 15177090 | caDSR Form |
Derived Variables
None
Process and Review
The PhenX Steering Committee (SC) reviewed this protocol in October 2023. Guidance from the SC includes:
- Updated protocol
Protocol Name from Source
National Health and Nutrition Examination Survey (NHANES), Anthropometry Procedures Manual, 2021-2023
Source
Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutritional Examination Survey (NHANES) 2021-2023. Anthropometry Procedures Manual (Section 3.4.8 - Abdominal (Waist) Circumference). Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
Certification for the Spanish translation can be found here.
General References
Because of the variability in the site of measurement of waist circumference, different cutoffs for metabolic syndrome in adults of various racial/ethnic groups, and variations among different populations of children and adolescents, more references are provided for potential users than for some other anthropometric measurements. Further, publications providing percentile curves (often including the 90th percentile) for children and adolescents have been included in the references as examples that may be suitable reference data for some investigations.
Alberti, K. G., Eckel, R. H., Grundy, S. M., Zimmet, P. Z., Cleeman, J. I., Donato, K. A., . . . Smith, S. C. (2009). Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation, 120(16), 1640-1645.
Brannsether, B., Roelants, M., Bjerknes, R., & Júlíusson, P. B. (2011). Waist circumference and waist-to-height ratio in Norwegian children 4-18 years of age: Reference values and cut-off levels. Acta Paediatrica, 100(12), 1576-82.
Bergen Growth Study, 2,945 boys and 2,780 girls, aged 4-18 years
Freedman, D. S., Serdula, M. K., Srinivasan, S. R., & Berenson, G. S. (1999). Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: The Bogalusa Heart Study. American Journal of Clinical Nutrition, 69(2), 308-317.
Galcheva, S. V., Iotova, V. M., Yotov, Y. T., Grozdeva, K. P., Stratev, V. K., & Tzaneva, V. I. (2009). Waist circumference percentile curves for Bulgarian children and adolescents aged 6-18 years. International Journal of Pediatric Obesity, 4(4), 381-388.
Bulgarian children, 2,052 boys and 1,758 girls, aged 6-18 years
Harrington, D. M., Staiano, A. E., Broyles, S. T., Gupta, A. K., & Katzmarzyk, P. K. (2012). Waist circumference measurement site does not affect relationships with visceral adiposity and cardiometabolic risk factors in children. Pediatric Obesity, 8(3), 199-206.
Jackson, R. T., Al Hamad, N., Prakash, P., & Al Somaie. M. (2011). Waist circumference percentiles for Kuwaiti children and adolescents. Public Health Nutrition, 14(1), 70-76.
Kuwait Nutrition Surveillance System (KNSS), schoolchildren, 4,843 boys and 4,750 girls, aged 5-18.9 years
Ji, C. Y., Yt Sung, R., Ma, G. S., Ma, J., He, Z. H., & Chen, T. J. (2010). Waist circumference distribution of Chinese school-age children and adolescents. Biomedical and Environmental Sciences, 23(1), 12-20.
Hong Kong and 15 mainland China provinces, 160,225 children and adolescents, aged 7-18 years
Kuriyan, R., Thomas, T., Lokesh, D. P., Sheth, N. R., Mahendra, A., Joy, R., . . . Kurpad, A. V. (2011). Waist circumference and waist for height percentiles in urban South Indian children aged 3-16 years. Indian Pediatrics, 48(10), 765-771.
PEACH (Pediatric Epidemiology and Child Health) Study, Bangalore, urban preschool- and school-age children, 5,172 boys and 3,888 girls, aged 3-16 years
Mancini, M. C. (2009). Metabolic syndrome in children and adolescents: Criteria for diagnosis. Diabetology & Metabolic Syndrome, 1, 20 doi:10.1186/1758-5996-1-20
Mason, C., & Katzmarzyk, P. T. (2009). Variability in waist circumference measurements according to anatomic measurement site. Obesity, 17(9), 1789-1795. doi:10.1038/oby.2009.87
Ross, R., Berentzen, T., Bradshaw, A. J., Janssen, I., Kahn, H. S., Katzmarzyk, P. T., . . . Després, J. P. (2008). Does the relationship between waist circumference, morbidity and mortality depend on measurement protocol for waist circumference? Obesity Reviews, 9(4), 312-325.
Samson, S. L., & Garber, A. J. (2014). Metabolic syndrome. Endocrinology Metabolism Clinics of North America, 43, 1-23.
World Health Organization. (2011). Waist circumference and waist-hip ratio: Report of a WHO expert consultation, Geneva, 8-11 December 2008. World Health Organization: Geneva.
Protocol ID
21604
Variables
Export Variables| Variable Name | Variable ID | Variable Description | dbGaP Mapping | |
|---|---|---|---|---|
| PX021604_Waist_Circumference_Waist_Circumference_Nhanes_Measurement | ||||
| PX021604010100 | Measured circumference at the top of the more | N/A | ||
Measure Name
Waist Circumference
Release Date
September 16, 2024
Definition
Waist circumference is a measurement to estimate the abdominal circumference.
Purpose
The measure of waist circumference is an indirect measure of abdominal fatness (central obesity), and a large waist circumference is associated with increased risk for diseases such as types 1 and 2 diabetes, dyslipidemia, hypertension, and cardiovascular disease. It is often used in conjunction with hip circumference to calculate the waist-to-hip ratio.
Keywords
Anthropometrics, abdominal obesity, obesity, weight, girth, Waist-To-Hip Ratio, WHR, Waist-to-Height Ratio, WtHR, metabolic syndrome, NHANES, NCFS
Measure Protocols
| Protocol ID | Protocol Name |
|---|---|
| 21602 | Waist Circumference - Waist Circumference NCFS |
| 21603 | Waist Circumference - Framingham Heart Study |
| 21604 | Waist Circumference - Waist Circumference NHANES |